Have you ever observed a young apparently healthy person using a wheelchair and see them stand up for a bit in a store? Your first thought is to wonder why they need a wheelchair at all. Today, learn about Dysautonomia– one of many chronic illnesses that make a wheelchair indispensable.
Recently, I caught up with a vibrant and positive former high school classmate and was surprised by all that she was patiently enduring with Dysautonomia. A relatively new chronic illness in her life just 5 years ago. This is one of those situations that, after learning about it, I hope I walk away a better person with a better sense of reality and empathy for others. To hear and absorb her story is to grow. The next time you see a seemingly healthy person using a wheelchair, you will have a better understanding and more compassion.
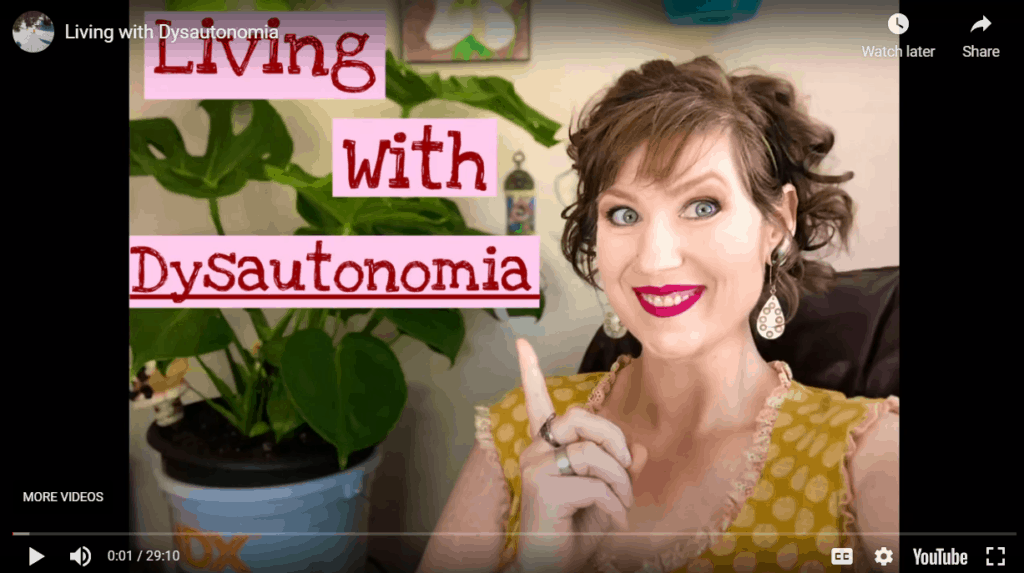
I have attached her full video recording which was a better medium for her to graciously answer the questions I asked from her. With a big thank you for her huge effort in this interview, read on to see through the lens of chronic illness.
This post contains Amazon affiliate links, which means I receive a small commission to put in the boat repair kitty, at no extra cost to you, if you make a purchase using links provided. Please see my disclosure page for more details.
Please introduce yourself to us
Hi, my name is Thea Sugarman Lee and I am 46 years old. I currently live in University Place, which is near Tacoma, WA… My chronic illness is actually Dysautonomic Syndrome and I’m going to read it for you because it’s a little complicated.

What chronic illnesses are you dealing with?
It’s called Neurogenic Orthostatic Hypotension with partial compensatory tachycardia, distal autonomic nervous neuropathy, and reduced sodomotor function distally.
So we break that down. Basically it just means that my brain is not working with my blood pressure and my heart. When I stand up my blood pressure likes to bottom out and my heart rate likes to spike. Or, sometimes my heart rate likes to go WAY down to maybe 50 beats per minute.
And then the distal autonomic nervous neuropathy just means that my hands and my feet are really numb. I’ve had to live with that for a very long time. Quite often I don’t feel burns on my hand if I’m cooking or getting something out of the oven. I have to be super careful when I do things like that. Be very aware.
Lastly, the sodomotor function distally basically just means that I’m not regulating my body temperature very well at all. So somebody who can go out when it’s hot and maybe sweat, I’m not able to do that. It will be mid-winter and all of a sudden I’m pouring sweat because I can’t regulate my body temperature. That’s kind of my diagnosis.
Will you tell us some of your hobbies, likes?
Absolutely! One of the fun things that I really like to do is travel. I’ve had some wonderful opportunities over the years to be able to travel all over the world. And it’s been so much fun. When I started getting really sick several years ago, I didn’t let it stop me from travelling. I thought maybe I could just push through it so I did do some traveling with a wheelchair. It takes a little more time, effort, accommodation, but it can be done.
I’ve definitely slowed down on that now. We just recently got back from Eastern Washington over the Cascade Mountains visiting family. That was a wonderful, beautiful way to experience the other side of the mountains. I actually traveled on an air mattress in the back seat.

Cooking with Dysautonomia
Oh, some of my other likes: I absolutely love to cook. I use to cook really foo-foo complicated food and I’m not longer able to do that so I’ve made some accommodations in my kitchen. I have a really super high bar stool, it’s actually higher than a normal bar stool. That allows me to sit at the stove and cook if need be, prep vegetables, or whatever needs to be at the counter top.
I also have a counter top convection oven that fits a 9×13 pan so I don’t have to bend over the oven. Of course, if I bend over chances are I’m probably going to fall into the oven and nobody really wants that… at least as far as I know. So, I’ve accommodated for that. I’ve introduced Intant Pots into our home cooking to make sure that we can get some really good, flavorful food so that I’m not actually having to sit, stir, and babysit. Because I just don’t have the energy to do that.
For the love of plants…
Lastly, I would say that one of my new favorite things to do in the last year and a half or so is to start caring for house plants. I found that I really missed being outside. I used to love to garden and I used to love to prepare the harvest vegetables by water bath canning, pressure canning, things like that. But, I’m not able to really do that without a lot of help anymore. House plants have been introduced into my home to bring the outside in because I pretty much am housebound.
I have lived in… well, I would say what people now call quarantine or self-isolation for that last 2 1/2 years. Very rarely do I leave the house so I needed something to bring the outside in and it’s been a joy to be able to do that.
Can you explain a little bit more about Dysautonomia Syndrome, what it’s like for you, how you learned that you had it? and the co-morbidities?
When our son (Sebastian who is now 21) was 3, I was in 2 car accidents 2 weeks apart. Neither one of them was my fault and both cars were totaled. Unfortunately, I ended up having 7 surgeries and procedures and was deemed 36% whole body impaired.
I lost my therapeutic massage career due to not being able to use my arms anymore. Several years after that, I was diagnosed with fibromyalgia. A couple of years after that, I was diagnosed with chronic fatigue. I had started getting some weird symptoms that really didn’t fit into “fibromyalgia’ or “chronic fatigue”. But, the doctors weren’t able to say what they were from.
Symptom clues
So, I would have postural hypotension which just means a lot of times you stand up too quickly and you have that moment of “whoa” (dizziness) and off you go. There were some other symptoms I had that were very mild with heart issues, heart racing, shortness of breath, things like that but they weren’t anything to be concerned about. It didn’t really fall into any categories.
When my husband needed to have a 2-part low back fusion, our son who was 15 at the time was struggling quite a bit as a high-functioning autistic guy. He had basically shut down and we were really struggling at how to help him the best that we could. When Richard had the surgery there were some complications and he ended up having to stay in the ICU and then instead of having an overnight visit it turned into a 5 day visit. We scrambled, thankfully we had a friend who was able to come and stay with Sebastian.

The Stress Toll Relationship with Dysautonomia
But, I was really torn: do I stay with my husband, do I stay with my son. My son needs me, he’s not doing well. My husband’s not doing well. What do I do? I’m not able to work, I’m scared, and it kind of triggered this emotional stress for me.
Three weeks later, he had to go in for the second part of the surgery and it was supposed to be just a day surgery. He had the surgery, we brought him home. Unfortunately, he had a really bad reaction. We tried taking him to the local ER, they ended up treating us very poorly, and we ended up having to scramble and take him to Seattle where he then spent another 5 days. Then we had to scramble yet again to find somebody to take care of Sebastian.
What is Dysautonomia?
The doctor believes (and it is the belief of those who diagnose Dysautonomic Sydrome) that emotional trauma or stress can actually trigger the symptoms and activate dysautonomia in your body.
If you break it down to it’s simplest terms, your autonomic nervous system is not communicating with the brain. The autonomic nervous system is responsible for so many of your body parts. The largest being that your gut is the largest part of the autonomic nervous system. Blinking of the eyes, your breathing, heart rate, blood pressure, it goes on and on.
Blood pooling is another major part– when you stand up, your brain is supposed to tell all of those veins in your legs to tighten up. When your brain forgets to tell your body to do that, the veins relax. Then all the blood just stays in the bottom of your body and doesn’t return. There’s a lot of things that can go wrong.
Co-Morbidities of Dysautonomia
I’m going to go ahead and read the list because I have quite a few co-morbidities. As you have this active chronic illness, co-morbidities just keep coming and you just have to keep managing the symptoms. There’s really nothing else that you can do. There’s no cure for Dysautonomia, there’s no cure for orthostatic hypotension. Let me go ahead and share with you what I deal with:
- I don’t regulate my body temperature
- Distal neuropathy
- Mast Cell Activation Syndrome: it’s actually the lesser, which there is a more severe called Mast Cell Activation Disorder. Broken down into the simplest terms is that my body just makes allergens. I’m basically allergic to my own body. There’s no rhyme or reason for me to have anaphylactic hives, or any other type of allergic reaction. My body just produces these reactions. So I live with that, it’s one of things you get to live with.
- Chronic migraines: chronic migraines are ones that you have more than 15 a month. I actually usually have 3 to 4 a week if not more.
- Chronic Fatigue Syndrome: it’s more on the severe side.
- Fibromyalgia. moderate to severe.
- Reduced sodomotor function distally.
- Severe blood pooling in my lower extremities, with all my extremities (a major part of Dysautonomia). My lower extremities are severe, my arms are moderate.
- Ehler Danlos Syndrome Type 3 which is a very mild form. Basically, a hypermobility of the musculoskeletal system. …
Gastroparesis and Dysautonomia
Gastroparesis is a condition where your stomach doesn’t empty. Food will actually sit in your stomach and your upper intestine for hours and hours. You get very nauseous, food doesn’t sit very well. You end up throwing up a lot. It doesn’t pass through so you get a lot of other unpleasant situations going on there.
For me it’s considered undiagnosed. Nine years ago I had gastric bypass due to some Type 2 Diabetes that ended up being insulin dependent. Meaning that the meds that I had for the Type 2 Diabetes no longer were working. My body was requiring insulin. So my endocrinologist had suggested gastric bypass which I went ahead and did.
Gastroparesis at the most severe stage, to help with it, they give you gastric bypass. The diagnostic tool that they use which is an emptying of the stomach test, I can’t do. I actually have all of the symptoms, deal with, and live with gastroparesis. But, they can’t give me an “official” diagnosis of it but they treat me just like I have it.
How do you manage the Dysautonomia?
There’s a lot. I have this thought process that the more tools that you have in your toolbox the better equipped you are to handle a new symptom coming in. I am not opposed to Western medicine, Eastern medicine, alternative care– I embrace it all because I truly believe that you have to treat the whole body.
- It’s really important for my mind to be in the right place so I am constantly making sure that I am reading back to myself positive things. Positive input gets positive output. That might sound hokey but I truly believe that it works.
- In addition, a full Western prescription of medications as well as a topical prescription cream that I take and I’m very thankful for it. It has helped me enormously and if it’s helpful, I’m never going to say no to it. If it gets to the point where it’s no longer helpful, I’m very happy to go off of it.
- Plethora of at home tools…a TENS unit which is electrical stimulation.
- Hot packs, cold packs
- I found this really neat thing called a Kailo patch online that actually works. It’s this neuroreceptor pain blocker.
- One of the biggest essential things is compression stockings for my blood pooling. They are 20-30 mmHg and I wear those everyday. It’s important to do that and I don’t go anywhere without them.
- I have an electric wheelchair for when I go out. I’m not able to walk for more than 2 or 3 minutes before my blood pressure bottoms out and my heart rate goes up. Sitting in a wheelchair is the best option for me.

Alternative Care
Alternative care: I see a massage therapist 2-4 times a month. He is fantastic, he actually does Wat Po Thai Massage which in Western Washington there are very few practitioners to offer this. Basically, it’s done with your clothes on. Using passive yoga stretches that he puts you in so that you’re not hurting yourself. Then he uses acupressure. On the off times, he uses Paul St. John’s neuromuscular re-education as well as a lot of different other techniques that go into a cervical massage… that help with stabilization and the migraines.
- Acupressure activator that’s manual and one that’s electric.
- Acupressure mat that I lay on that’s just this pad. It’s got these really super spiky hard flowers that come out. You lay on it and it helps stimulate those acupressure points.
- I also listen to hertz sounds at different vibrations to help with that. If you look into any Tibetan Singing Bowls or anything like that, it’s really an interesting study.

Natural Health Supplements
- Lovely amount of supplements in my foods as well as by mouth. A 10-blend mushroom powder, teas like Pu-erh and Rooibos for inflammation. Moringa leaf, steeped and used for energy. Multi-vitamin that has pre-biotics, pro-biotics, omegas, all the organic good stuff.
- Apple Cider Vinegar tablets
- Lots of water: 3 to 4 full water bottles a day. (See video for size)
- Arnica Oil: I rub it all over. Also, I take Arnica tablets.
Best Care Option That I’ve Recently Added:
A permanent port! You can’t really see it but it’s a little, hard, round silicone..(see video for placement). It’s got a hose/tube/catheter that goes in and I get a liter of IV saline infusions daily, Monday through Thursday. On Fridays, I get 2 liters of saline. It takes about 4 hours for 1 liter of saline to go through. Once a week I have a home health nurse come and put in my catheter and get me ready for the week.

What does a typical day look like or do you have typical days with Dysautonomia?
Well, that’s a good question. I think it really depends on the time of year. We live in Western Washington and unfortunately, for most of the year it’s kind of wet, cold, damp and those REALLY bother my body so much and it drains my energy. It just makes me feel really yucky. Those kinds of day I’ll see increases of migraines, pain, and decrease of energy levels. I will spend the majority of my time in bed.
On summer days like now, it’s the most glorious time for me. The sun is out, the weather is not overly hot and I can be out. My energy levels are a little bit more.
So on good days I love to come out into my living room, enjoy/ talk to my husband and my son if they’re here. Read on my Kindle if nobody is here. Visit online with my social media, I have a close support group and chat with.
The typical day, I don’t leave the house very often. I truly am pretty much housebound.
What is something you wish that other people knew about your Dysautonomia and other conditions?
I think the biggest thing that I would like for people to truly understand is that chronic is long-term. It’s so beautiful when people have that compassion and kindness. When they first see and understand they have this well of compassion for you right away and it’s so beautiful then pretty soon it gets out of sight, out of mind. The next time they see you they’re kindof confused and scratching their head thinking, “you’re still dealing with this?” It’s like, “Yah, chronic means really super long time if not forever.”
Now, I am open to a miracle. IF God wanted to heal me, I am open to it. Please, I’m ready! BUT, if He chooses not to, if I live with this, that’s ok, too. That just means that I have to manage it.
Chronic means long-term and I would much rather have somebody come over for a quick visit. Even if I’m in my jammy-jams and I haven’t showered for 2 weeks because I don’t have the energy to get out of bed and visit because there’s nothing as heart-warming and beautiful than to be remembered.
It’s too difficult to ask and expect people to come to your house and pick you up, put your 50 pound wheelchair into their car. When you get someplace to take it out and when you’re done put it back in. When you get home, unload it. That A LOT! That’s a big commitment for anybody. You learn that it just isn’t always feasible. That doesn’t mean that the person doesn’t care, it doesn’t mean that the person doesn’t love you. It just means that it isn’t workin’.
I live my life virtually pretty much online and love having a social media platform where I can share what my life is like.

Are there any bucket-list items or goals that you have for this coming year?
I think the biggest thing that I’m really thinking about, we’re right in the midst of Covid and it’s very interesting because I’ve been living a self-isolated quarantine lifestyle with Dysautonomia for a couple years where I have my delivery of groceries come and I don’t go anywhere. It’s been very difficult on other people. I’ve tried to start to do some encouraging little Instagram posts when the quarantine started. Just maybe some tips and tricks or encouraging words. I would like to just continue to share on my social media platform. Allow that to be a place where people can understand and get a true realistic look at what life can be like with somebody who has a chronic illness.
The good days, the bad days, the frustrating days. I am really appreciating the wonderful reception that I have gotten on social media.
Thank you so much. If you have any comments or questions about chronic illnesses mentioned or Dysautonomia please feel free to leave a comment on my video.
I am so thankful to Thea for taking the time and effort to detail what it is like to live with Dysautonomia and chronic illness. We are all blessed to learn more how to understand and interact in this type of situation. To be completely frank, when someone is suffering or dealing with issues we don’t quite understand, we don’t always know what to say or do. So, we don’t and avoid the situation. I appreciate the tip on what would really be helpful to you.
Do you have a chronic illness? What is a helpful tip for let others know how to interact? Feel free to comment below.